
Altering the appearance of macrophages to prevent atherosclerosis
It might be possible to prevent atherosclerosis by changing the appearance of macrophages, cells of the immune system that for example digest foreign substances. In her PhD dissertation, Baoyan Ren examined several ways to do so.
Fat-laden foam cells
In atherosclerosis, Ren explains, macrophages accumulate cholesterol. This leads to their transformation into foam cells. These fat-laden cells cause arterial narrowing and hardening, with an increased risk of heart attack and stroke for the patient.
New targets for drugs
Statins are medicines that can lower cholesterol levels and can thus slow down the development of atherosclerosis. Ren says: ‘These drugs are not effective enough to decrease the high incidence of atherosclerosis-induced cardiovascular disease. That’s why we’re looking hard for new targets suitable for drug development against the disease.’
Inflammation and atherosclerosis
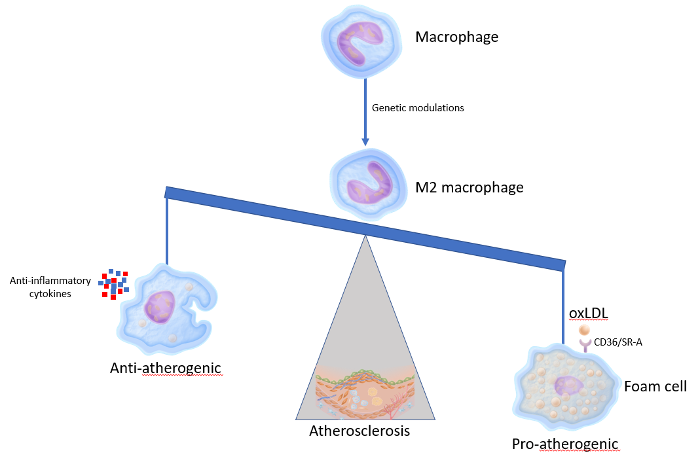
Atherosclerosis is a classic inflammation-driven disease. Inflammation plays a major role in all phases of promoting the disease. Ren: ‘Atherosclerosis causes damage to the inside of the arteries. In these lesions, two major types of macrophages can be distinguished: pro-inflammatory M1-macrophages, which promote atherosclerosis, and anti-inflammatory M2-macrophages, which protect against the formation of atherosclerosis. Inducing M1-macrophages to M2-macrophages may be a promising approach to protect against this disease.’
Foam cell formation
By examining several genes, Ren was successful in altering macrophages into an M2-phenotype, hoping to prevent the formation of atherosclerosis. Alas, this also led to accelerated foam cell formation, she found out.
This is caused by the uptake of proteins called oxLDL, oxidized Low Density Lipoproteins. These proteins transport fat and are recognised by different receptors. Ren identified the two main receptors that are responsible for almost 90 percent of the oxLDL uptake.
M2 macrophage cells highly express these two receptors compared with M1 macrophage cells. Therefore skewing M1 macrophages to a M2 phenotype leads to accelerated foam cell formation. This counteracted the protective effects of the M2-macrophage, thereby limiting its therapeutic value.
Ren: ‘Skewing M1 macrophages to the M2 phenotype with plasma cholesterol-lowering drugs might be an alternative therapeutic strategy for atherosclerosis, and hence against cardiovascular disease. However, more research is required to identify the key beneficial regulators and their overall effects. It would be interesting to evaluate whether selective targeting of macrophage polarization is indeed an effective approach for the treatment of atherosclerosis and for the reduction of cardiovascular risk.’
